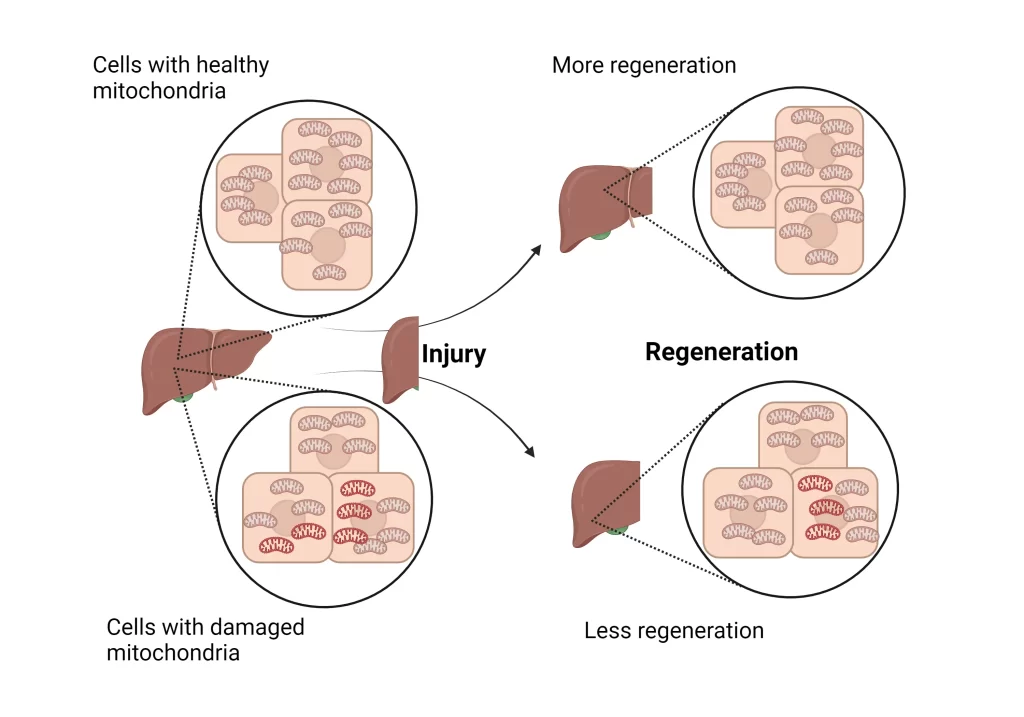
According to the CDC (Centers for Disease Control and Prevention), liver disease is at 10th rank for the cause of death in the United States. In human liver diseases– liver failure, cirrhosis, and fatty liver– the liver regeneration capacity is reduced but we do not know how. Past studies have shown that damaged mitochondria are present in liver cells in these diseases. This motivated the scientists to find out how damaged mitochondria could affect liver regeneration
What did they do?
The scientists worked on mice to surgically remove 70% of their liver, forcing it to regenerate. They measured various metabolite levels in mitochondria to know which nutrients were used during regeneration. They observed lower fatty acid levels, due to increased fatty acid digestion of fats in the food. As a next step, they aimed to measure these levels in damaged mitochondria. To create damaged mitochondria, they mutated different genes of the electron transport chain (ETC). ETC is a pathway that generates energy in mitochondria. It is indirectly required for fatty acid digestion. Consequently, they observed reduced fatty acid digestion — or, increased fatty acid levels — that decreased liver regeneration. To confirm the role of fatty acids, they used chemical/genetic manipulation to increase fatty acid digestion in the damaged mitochondria. They found a subsequent increase in liver regeneration, hoping to use it as a potential treatment. Based on these findings they concluded that damaged mitochondria reduced liver regeneration by decreasing fatty acid digestion. Thereby allowing cells with healthy mitochondria to grow more, contributing to regeneration. This is a good example of natural selection at a cellular level to promote a healthy organ.
What are the next steps?
This study demonstrated that increasing fatty acid oxidation in damaged mitochondria improves mice’s liver regeneration ability. The next step would be to test these therapies in mouse liver disease models, which would mimic human disease. Other large animal models should also be used to validate these therapies. The ultimate test would be in clinical trials to know their efficacy and safety in humans. However, getting approval for clinical trials is a long process with multiple steps that could take several years.
How does this research affect humans?
In liver diseases, where most of the mitochondria are damaged, the liver is unable to rejuvenate. Therapies that increase fatty acid digestion can be used based on this study. However, patients with liver diseases have different underlying causes. These therapies could work only on those patients who have high fatty acid levels in their liver cells’ mitochondria. Thus, to determine who would respond to these drugs, patients’ biopsies need to be performed to measure mitochondria fatty acid levels. This study opens new directions to treat liver diseases, whose potential needs to be further verified.
More detail The research article was published in Science journal on June 14th 2024 and is available here.